If left untreated, late-stage ocular surface squamous neoplasia (OSSN) can lead to devastating consequences, including disfigurement, intraocular extension, and metastases. (See “OSSN: An Overview”.) Therefore, it is imperative that corneal specialists accurately diagnose and effectively treat the condition.
Here, we explain how this can be accomplished.
Accurate Diagnosis
The presenting symptoms of OSSN can be complaints of varying degrees of ocular irritation, redness, and visual impairment.1 Alternatively, OSSN patients can present without symptoms, underscoring the importance of a routine, comprehensive examination.
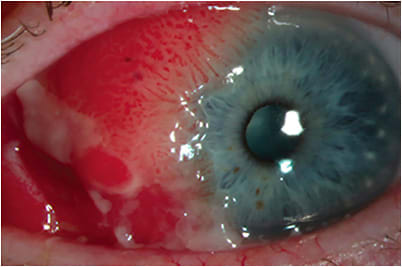
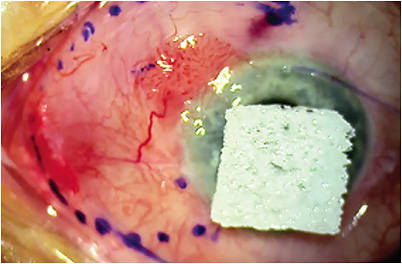
Slit lamp exam commonly reveals fleshy lesions that have leukoplakic, papillomatous (see Figure 1), or gelatinous qualities.2 OSSN lesions may be further highlighted using lissamine green, Rose Bengal, and methylene blue stains.3 Further, the interpalpebral conjunctiva is the most affected site.1,3
These clinical findings can be elucidated with the following imaging modalities:
- HR-OCT. This is highly sensitive and specific for the diagnosis. OSSN specifically has a characteristic appearance of abnormally thickened and hyperreflective epithelium, arising from an abrupt transition from normal epithelium.4,5
- In vivo confocal microscopy. This may reveal cells that have atypical features, such as high nuclear to cytoplasmic ratio, pleomorphism, or active mitosis.6,7
- Exfoliative cytology. This allows for the examiner to sample superficial tissue for microscopic analysis. The results can be comparable to histopathology with regard to malignant tissue.8However, it cannot replace excisional biopsy.9
Clinical diagnosis alone is accurate between 40% to 86% of the time.1,10 The gold standard for a definitive diagnosis is histopathology following excisional biopsy.11
Effective Treatment
Surgical excision, topical agents (either in combination with surgery or as monotherapy), and alternative therapeutic options are available to treat OSSN:
- Surgical excision. Typically, this involves a no-touch technique with 4 mm margins, followed by cryotherapy via the double-freeze slow-thaw technique and/or application of absolute alcohol (see Figure 2).12 Closure can occur via primary wound closure for smaller wounds, while amniotic membrane closure may be employed for larger wounds (see Figure 3).13
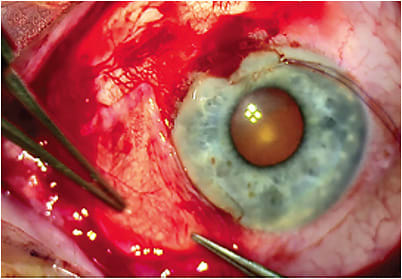
Of note: Partial lamellar sclerectomy,14 enucleation,15 or exenteration16,17 could be considered for significantly advanced forms of OSSN, or for lesions that involve scleral, intraocular, or orbital invasion.
Benefits. These include the certainty of removing clinically obvious lesions, the ability to determine a specific diagnosis with histopathology, and shortening the overall timeframe for treatment.13
Drawbacks. Conjunctival scarring, symblepharon, and conjunctival hyperemia are possible sequelae.2,18 Additionally, depending on the location of the lesion, some degree of limbal stem cell deficiency may be present.19 Further, OSSN has been recognized as a multifocal disease that may not be adequately managed with surgery alone.19,20 Finally, the recurrence rate of OSSN following surgical excision can be up to 56%.1,21
- Topical agents. Topical immunomodulating (i.e., interferon alfa-2b) and chemotherapeutic agents (i.e., 5-fluorouracil and mitomycin C) can treat the entire ocular surface, ostensibly minimizing the area for surgical resection and treating subclinical disease. HR-OCT can potentially minimize disease recurrence here by either aiding in the confirmation of disease resolution or revealing subclinical OSSN in eyes that would benefit from extended topical therapy.22Interferon alfa-2b benefits. This immunomodulatory cytokine works to protect against microbes and viruses. It has an efficacy rate of up to 100%,23 can be used topically or as a subconjunctival injection, and causes few side effects.
Interferon alfa-2b drawbacks. This medication must be refrigerated, and it’s hard to come by. Since the COVID-19 pandemic, the sole manufacturer discontinued it “for business reasons,” so the existing supply continues to dwindle. Dosing is typically daily, with each cycle spanning 4 weeks.
5-fluorouracil benefits. This chemotherapeutic agent interrupts DNA formation.
5-fluorouracil drawbacks. Side effects may include ocular surface irritation, filamentary keratitis, and superficial stromal melting. Dosing is typically 4 times daily for 1 week to 2 weeks, with a drug holiday of 2 weeks to 4 weeks.
Mitomycin C benefits. This chemotherapeutic agent inhibits RNA and protein synthesis. It also has an efficacy rate of up to 100%.24
Mitomycin C drawbacks. It poses a risk of ocular surface toxicity and can cause hyperemia, conjunctivitis, and punctal stenosis. (Punctal plugs are placed by some providers to reduce punctal damage.) Dosing is typically 4 times daily for 1 week to 2 weeks, with a drug holiday of 2 weeks to 4 weeks. - Alternative therapeutic options. These include photodynamic therapy (PDT), radiation, anti-VEGF agents, human papillomavirus vaccinations, and Aloe vera.PDT benefits. This uses photosensitive agents to convert light into chemical reactions, resulting in the release of free radicals and offering a targeted option against malignant cells that limits the destruction of surrounding healthy tissue.
PDT drawbacks. There are limited studies on its use in OSSN.25
Radiation benefits. This treatment, which kills and hampers cancer cell growth via DNA damage, has been described as an adjuvant to surgery and can come in various forms, such as proton radiation, electron beam radiation, brachytherapy, stereotactic radiotherapy, etc.26 The type of radiation used may depend on the extent of the disease.
For example, electron beam radiation has been highlighted in a case report of OSSN with orbital extension.26 In less invasive cases, such as in OSSN that has scleral involvement, brachytherapy can be considered.27
Radiation drawbacks. Depending on the type of radiotherapy and treatment location, patients may develop persistent epithelial defects,27 corneal ulceration, and limbal stem cell deficiency.28
Anti-VEGF benefits. Limited studies demonstrate improved vascularity and size following treatment with topical or subconjunctival bevacizumab.29,30
Anti-VEGF drawbacks. Use of these agents in the presence of an epithelial defect may prevent corneal wound healing.31
HPV vaccination benefits. They may potentially lend themselves to novel immunomodulatory therapies against ocular surface neoplasias, as suggested in the case of a conjunctival papilloma refractory to 5-fluorouracil that subsequently responded to two vaccinations.32 Although HPV is not required for OSSN development, it is thought to play a role in a subset of OSSN cases, with groups theorizing that widespread vaccination could prevent future OSSN cases.33 Studies are currently underway to explore the potential of this as an intervention.34
Aloe vera benefits. This antineoplastic plant that has anti-inflammatory properties is credited with the resolution of OSSN in one published case report, in which the patient had begun using topical aloe vera drops resulting in the disappearance of her lesion within three months of treatment initiation.35
Aloe vera drawbacks. Further studies are needed to confirm whether aloe vera has utility against OSSN.

A Call to Action
Because unidentified and untreated OSSN can cause disfigurement, intraocular extension, and metastases, it’s crucial that corneal specialists be aware of the condition’s characteristics, employ the necessary diagnostic technology to aid in detection, perform histopathology following excisional biopsy for a definitive diagnosis, and treat the condition using surgery, topical agents, or alternative therapeutic options. Overall, the process of deciding among management approaches should include considerations of cost, patient compliance, and patient preference. CP
References:
- Tabin G, Levin S, Snibson G, Loughnan M, Taylor H. Late recurrences and the necessity for long-term follow-up in corneal and conjunctival intraepithelial neoplasia. Ophthalmology. 1997;104(3):485-492.
- Kaliki S, Kamal S, Fatima S. Ocular surface squamous neoplasia as the initial presenting sign of human immunodeficiency virus infection in 60 Asian Indian patients. Int Ophthalmol. 2017;37(5):1221-1228.
- Sayed-Ahmed IO, Palioura S, Galor A, Karp CL. Diagnosis and medical management of ocular surface squamous neoplasia. Expert Rev Ophthalmol. 2017;12(1):11-19.
- Karp CL, Scott IU, Chang TS, Pflugfelder SC. Conjunctival intraepithelial neoplasia. A possible marker for human immunodeficiency virus infection? Arch Ophthalmol. 1996;114(3):257-261.
- Lee GA, Hirst LW. Ocular surface squamous neoplasia. Surv Ophthalmol. 1995;39(6):429-450.
- Kieval JZ, Karp CL, Shousha MA, et al. Ultra-high resolution optical coherence tomography for differentiation of ocular surface squamous neoplasia and pterygia. Ophthalmology. 2012;119(3):481-486.
- Venkateswaran N, Mercado C, Wall SC, Galor A, Wang J, Karp CL. High resolution anterior segment optical coherence tomography of ocular surface lesions: A review and handbook. Expert Rev Ophthalmol. 2021;16(2):81-95.
- Nguena MB, van den Tweel JG, Makupa W, et al. Diagnosing ocular surface squamous neoplasia in East Africa: case-control study of clinical and in vivo confocal microscopy assessment. Ophthalmology. 2014;121(2):484-491.
- Xu Y, Zhou Z, Xu Y, Liu F, Qu H, Hong J. The clinical value of in vivo confocal microscopy for diagnosis of ocular surface squamous neoplasia. Eye (Lond). 2012;26(6):781-787.
- Kayat KV, Correa Dantas PE, Felberg S, Galvão MA, Saieg MA. Exfoliative cytology in the diagnosis of ocular surface squamous neoplasms. Cornea. 2017;36(1):127-130.
- Semenova EA, Milman T, Finger PT, et al. The diagnostic value of exfoliative cytology vs histopathology for ocular surface squamous neoplasia. Am J Ophthalmol. 2009;148(5):772-778.
- Kao AA, Galor A, Karp CL, Abdelaziz A, Feuer WJ, Dubovy SR. Clinicopathologic correlation of ocular surface squamous neoplasms at Bascom Palmer Eye Institute: 2001 to 2010. Ophthalmology. 2012;119(9):1773-1776.
- Adler E, Turner JR, Stone DU. Ocular surface squamous neoplasia: a survey of changes in the standard of care from 2003 to 2012. Cornea. 2013;32(12):1558-1561.
- Shields JA, Shields CL, De Potter P. Surgical management of conjunctival tumors. The 1994 Lynn B. McMahan Lecture. Arch Ophthalmol. 1997;115(6):808-815.
- Yeoh CHY, Lee JJR, Lim BXH, et al. The management of ocular surface squamous neoplasia (OSSN). Int J Mol Sci. 2022;24(1):713.
- Buuns DR, Tse DT, Folberg R. Microscopically controlled excision of conjunctival squamous cell carcinoma. Am J Ophthalmol. 1994;117(1):97-102.
- Shields JA, Shields CL, Gunduz K, Eagle RC Jr. The 1998 Pan American Lecture. Intraocular invasion of conjunctival squamous cell carcinoma in five patients. Ophthalmic Plast Reconstr Surg. 1999;15(3):153-160.
- Rajabi MT, Ghasemi H, Safizadeh M, et al .Conjunctival squamous cell carcinoma with intraocular invasion after radiotherapy in epidermodysplasia verruciformis. Can J Ophthalmol. 2014;49(2):e43-e46.
- Nanji AA, Moon CS, Galor A, Sein J, Oellers P, Karp CL. Surgical versus medical treatment of ocular surface squamous neoplasia: a comparison of recurrences and complications. Ophthalmology. 2014;121(5):994-1000.
- Hirst LW. Randomized controlled trial of topical mitomycin C for ocular surface squamous neoplasia: early resolution. Ophthalmology. 2007;114(5):976-982.
- Besley J, Pappalardo J, Lee GA, Hirst LW, Vincent SJ. Risk factors for ocular surface squamous neoplasia recurrence after treatment with topical mitomycin C and interferon alpha-2b. Am J Ophthalmol. 2014;157(2):287-293.
- Tran AQ, Venkateswaran N, Galor A, Karp CL. Utility of high-resolution anterior segment optical coherence tomography in the diagnosis and management of sub-clinical ocular surface squamous neoplasia. Eye Vis (Lond). 2019;6:27.
- Galor A, Karp CL, Chhabra S, Barnes S, Alfonso EC. Topical interferon alpha 2b eye-drops for treatment of ocular surface squamous neoplasia: a dose comparison study. Br J Ophthalmol. 2010;94(5):551-554.
- Nanji AA, Sayyad FE, Karp CL. Topical chemotherapy for ocular surface squamous neoplasia. Curr Opin Ophthalmol. 2013;24(4):336-342.
- Cekiç O, Bardak Y, Kapucuoğlu N. Photodynamic therapy for conjunctival ocular surface squamous neoplasia. J Ocul Pharmacol Ther. 2011;27(2):205-207.
- Murthy R, Gupta H, Krishnatry R, Laskar S. Electron beam radiotherapy for the management of recurrent extensive ocular surface squamous neoplasia with orbital extension. Indian J Ophthalmol. 2015;63(8):672-674.
- Arepalli S, Kaliki S, Shields CL, Emrich J, Komarnicky L, Shields JA. Plaque radiotherapy in the management of scleral-invasive conjunctival squamous cell carcinoma: an analysis of 15 eyes. JAMA Ophthalmol. 2014;132(6):691-696.
- Faramarzi A, Feizi S. Subconjunctival bevacizumab injection for ocular surface squamous neoplasia. Cornea. 2013;32(7):998-1001.
- Özcan AA, Çiloğlu E, Esen E, Şimdivar GH. Use of topical bevacizumab for conjunctival intraepithelial neoplasia. Cornea. 2014;33(11):1205-1209.
- Sripawadkul W, AlBayyat G, Galor A, et al. Resolution of a presumed conjunctival papilloma after therapeutic treatment with the human papillomavirus vaccine. JAMA Ophthalmol. 2022;140(4):434-435.
- Carroll JN, Willis ZI, de St Maurice A, Kohanim S. Human papilloma virus vaccination and incidence of ocular surface squamous neoplasia. Int Ophthalmol Clin. 2017;57(1):57-74.
- Mott M. New approaches with OSSN. Eyenet. 2022;26(11):38-44.
- Damani MR, Shah AR, Karp CL, Orlin SE. Treatment of ocular surface squamous neoplasia with topical Aloe vera drops. Cornea. 2015;34(1):87-89.
- Dalvin LA, Salomão DR, Patel SV. Population-based incidence of conjunctival tumours in Olmsted County, Minnesota. Br J Ophthalmol. 2018;102(12):1728-1734.
- Höllhumer R. Ocular manifestations of hydroa vacciniforme in a Black child. Eur J Ophthalmol. 2020;30(2):NP32-NP34.
- Porges Y, Groisman GM. Prevalence of HIV with conjunctival squamous cell neoplasia in an African provincial hospital. Cornea. 2003;22(1):1-4.
- Makupa II, Swai B, Makupa WU, White VA, Lewallen S. Clinical factors associated with malignancy and HIV status in patients with ocular surface squamous neoplasia at Kilimanjaro Christian Medical Centre, Tanzania. Br J Ophthalmol. 2012;96(4):482-484.
- Kamal S, Kaliki S, Mishra DK, Batra J, Naik MN. Ocular surface squamous neoplasia in 200 patients: a case-control study of immunosuppression resulting from human immunodeficiency virus versus immunocompetency. Ophthalmology. 2015;122(8):1688-1694.
- Lee GA, Hirst LW. Incidence of ocular surface epithelial dysplasia in metropolitan Brisbane. A 10-year survey. Arch Ophthalmol. 1992;110(4):525-527.
- Gichuhi S, Sagoo MS, Weiss HA, Burton MJ. Epidemiology of ocular surface squamous neoplasia in Africa. Trop Med Int Health. 2013;18(12):1424-1443.
- Newton R, Ziegler J, Ateenyi-Agaba C, et al; Uganda Kaposi's Sarcoma Study Group. The epidemiology of conjunctival squamous cell carcinoma in Uganda. Br J Cancer. 2002;87(3):301-308.
- Nakamura Y, Mashima Y, Kameyama K, Mukai M, Oguchi Y. Detection of human papillomavirus infection in squamous tumours of the conjunctiva and lacrimal sac by immunohistochemistry, in situ hybridisation, and polymerase chain reaction. Br J Ophthalmol. 1997;81(4):308-313.
- Napora C, Cohen EJ, Genvert GI, et al. Factors associated with conjunctival intraepithelial neoplasia: a case control study. Ophthalmic Surg. 1990;21(1):27-30.
- Basti S, Macsai MS. Ocular surface squamous neoplasia: a review. Cornea. 2003;22(7):687-704.

DR. TRAN is an ophthalmology resident in the Department of Ophthalmology at Harvard Medical School. She has been published in multiple peer-reviewed journals, including Investigative Ophthalmology and Visual Science, Cornea, Scientific Reports, and Experimental Eye Research. Additionally, she has presented her work at various conferences, such as ARVO, the Biennial Cornea Conference, and the American Medical Women’s Association.

DR. VENKATESWARAN practices at Massachusetts Eye and Ear Harvard Medical School Department of Ophthalmology, where she is also an instructor. Her specialties are complex and premium cataract surgery, cornea and external diseases, corneal crosslinking, and refractive surgery. She is a consultant for CorneaGen.